
Find Effective Menstrual Cramps Relief with Herbal Tea Tips
Effective Menstrual Cramps Relief: Heating Pads, Herbal Teas, and Proven Pain Solutions

Menstrual cramps relief combines targeted therapies, from heat application to herbal infusions, to soothe uterine contractions and ease daily discomfort. Whether you reach for a heating pad for period pain, brew herbal tea for cramps, or rely on over-the-counter medication, understanding the underlying causes and mechanisms empowers you to choose the fastest, safest, and most sustainable solutions. This guide covers:
- What causes menstrual cramps and how they influence pain
- Rapid relief with heating pads and heat patches
- Optimal over-the-counter pain relievers
- Natural remedies and herbal teas
- Dietary shifts and supplements for sustained support
- Exercises and lifestyle changes for prevention
- Advanced medical treatments for severe or secondary cramps
What Causes Menstrual Cramps and How Do They Affect Pain Levels?
Menstrual cramps (dysmenorrhea) stem from elevated prostaglandin levels triggering uterine contractions that compress blood vessels and stimulate pain-sensing nerves. This biochemical cascade amplifies discomfort, influencing cramp intensity, duration, and associated symptoms.
Prostaglandins, the lipid compounds produced by the uterine lining, coordinate contraction strength. When levels peak, the uterus tightens vigorously to shed its lining, leading to sharp or throbbing pelvic pain. Individual factors—hormonal fluctuations, inflammation, and underlying conditions—determine why some individuals experience mild discomfort while others face severe cramps.
These biochemical and physiological processes set the stage for selecting targeted relief strategies that interrupt prostaglandin activity or counteract muscle tension.
What role do prostaglandins play in causing period pain?
Prostaglandins are signaling molecules produced in the uterine lining that orchestrate the rhythmic contractions responsible for shedding uterine tissue. High prostaglandin concentrations intensify uterine muscle contractions and reduce local blood flow, triggering spasms and hypoxia. Inhibiting prostaglandin synthesis directly lessens contraction severity, which underlies the efficacy of NSAIDs like ibuprofen.
Prostaglandins and Menstrual Cramps
Prostaglandins, produced in the uterine lining, are key in causing menstrual cramps by triggering uterine contractions and reducing blood flow. High levels of these compounds intensify muscle contractions, leading to pain and discomfort during menstruation.
Dawood, M. Y., Dysmenorrhea and Prostaglandins: A Review (1981)
This research explains the role of prostaglandins in causing period pain, which is a central topic in the article.
How do primary and secondary dysmenorrhea differ in symptoms and causes?
Primary dysmenorrhea refers to no-pathology period pain driven by cyclic prostaglandin release and normal ovulatory cycles. It typically begins shortly before or at menstrual onset and improves with age or after childbirth. Secondary dysmenorrhea involves underlying conditions—such as endometriosis, fibroids, or pelvic inflammatory disease—that cause persistent or progressively worsening cramps, often accompanied by abnormal bleeding or pain between cycles.
When should you seek medical help for severe menstrual cramps?
Seek medical attention if cramps persist beyond several days, intensify over successive cycles, or disrupt daily activities despite self-care. Warning signs include debilitating pain unrelieved by NSAIDs, heavy menstrual bleeding, fever, or gastrointestinal symptoms. Early evaluation rules out secondary dysmenorrhea and guides interventions like hormone therapy or surgical management when necessary.
How Can Heating Pads Provide Fast and Effective Relief for Period Pain?

Heat therapy relaxes uterine muscles and increases pelvic blood flow, interrupting the prostaglandin-driven contraction cycle. A heating pad for period pain delivers sustained warmth that soothes muscle spasms, reduces inflammatory mediators, and prompts endorphin release, offering relief within minutes.
Benefits of Heat Therapy for Menstrual Cramps
Heat therapy is effective for menstrual cramps because it relaxes uterine muscles and increases pelvic blood flow. This process helps to interrupt the cycle of prostaglandin-driven contractions, providing relief from pain and discomfort.
French, L., Dysmenorrhea (2005)
This research supports the article's claims about the benefits of heat therapy for menstrual cramps.
Using a heating pad prior to peak cramp onset can prevent tension buildup and minimize analgesic reliance. Incorporating targeted heat as a first-line remedy grounds subsequent pain management strategies in natural muscle relaxation.
What are the benefits of heat therapy for menstrual cramps?
Before exploring pad types, consider these core benefits:
| Entity | Attribute | Value |
|---|---|---|
| Heat Therapy | Mechanism | Increases local blood flow and relaxes muscles |
| Uterine Muscle Spasms | Benefit | Reduced contraction intensity and duration |
| Pain Perception | Outcome | Elevated endorphin release lowers pain sensation |
| Inflammatory Mediators | Effect | Decreased prostaglandin concentration |
How to use heating pads safely and effectively during menstruation?
Before applying heat, ensure skin protection by wrapping a pad in a thin cloth to avoid burns. Follow these steps:
- Preheat the pad according to manufacturer instructions.
- Position on the lower abdomen or lower back where cramping is most intense.
- Use intermittent cycles: 20 minutes on, 10 minutes off to prevent overheating.
- Combine with light stretching or relaxation breathing to enhance muscle relaxation.
Consistent, safe application supports sustained relief and prevents skin irritation, paving the way for seamless integration with other remedies.
What types of heating pads and heat patches are best for period pain?
Different devices suit varied preferences:
| Product Type | Feature | Benefit |
|---|---|---|
| Electric Heating Pad | Adjustable temperature | Customizable warmth for targeted comfort |
| Microwavable Wrap | Portable, reusable | On-the-go relief without plugs |
| Adhesive Heat Patch | Continuous low heat (8+ hrs) | Discreet, long-lasting muscle relaxation |
| Heat Belt | Full lumbar coverage | Simultaneous abdominal and back relief |
Which Over-the-Counter Pain Relievers Work Best for Menstrual Cramps?
NSAIDs like ibuprofen and naproxen inhibit prostaglandin synthesis to address the root cause of cramps. By targeting cyclooxygenase (COX) enzymes, they reduce inflammatory mediators and uterine contractions, delivering rapid pain relief.
How do NSAIDs like ibuprofen and naproxen relieve menstrual pain?
NSAIDs block COX-1 and COX-2 enzymes responsible for converting arachidonic acid into prostaglandins. Lower prostaglandin levels translate to fewer uterine spasms and diminished pain signals.
| Drug | Mechanism | Onset | Common Use |
|---|---|---|---|
| Ibuprofen | COX inhibition → ↓ Prostaglandins | 30–60 minutes | Mild to moderate cramps |
| Naproxen | Prolonged COX inhibition | 60–90 minutes | Longer relief for sustained pain |
| Aspirin | Nonselective COX inhibition | 30–60 minutes | Occasional use when NSAID-tolerant |
What are the recommended dosages and side effects of common OTC painkillers?
- Ibuprofen: 200–400 mg every 4–6 hours (max 1200 mg/day).
- Naproxen: 220 mg every 8–12 hours (max 660 mg/day).
- Aspirin: 325–650 mg every 4 hours (max 4000 mg/day).
Common side effects include gastrointestinal upset, heartburn, and rare risks of bleeding. Taking NSAIDs with food and hydration minimizes adverse reactions and supports continued use.
Can acetaminophen be used for menstrual cramps relief?
Yes, acetaminophen reduces pain by blocking central pain pathways but does not inhibit prostaglandins peripherally. It offers moderate relief for individuals unable to tolerate NSAIDs, though pairing with heat therapy often enhances overall comfort.
What Natural Remedies and Herbal Teas Help Alleviate Menstrual Cramps?

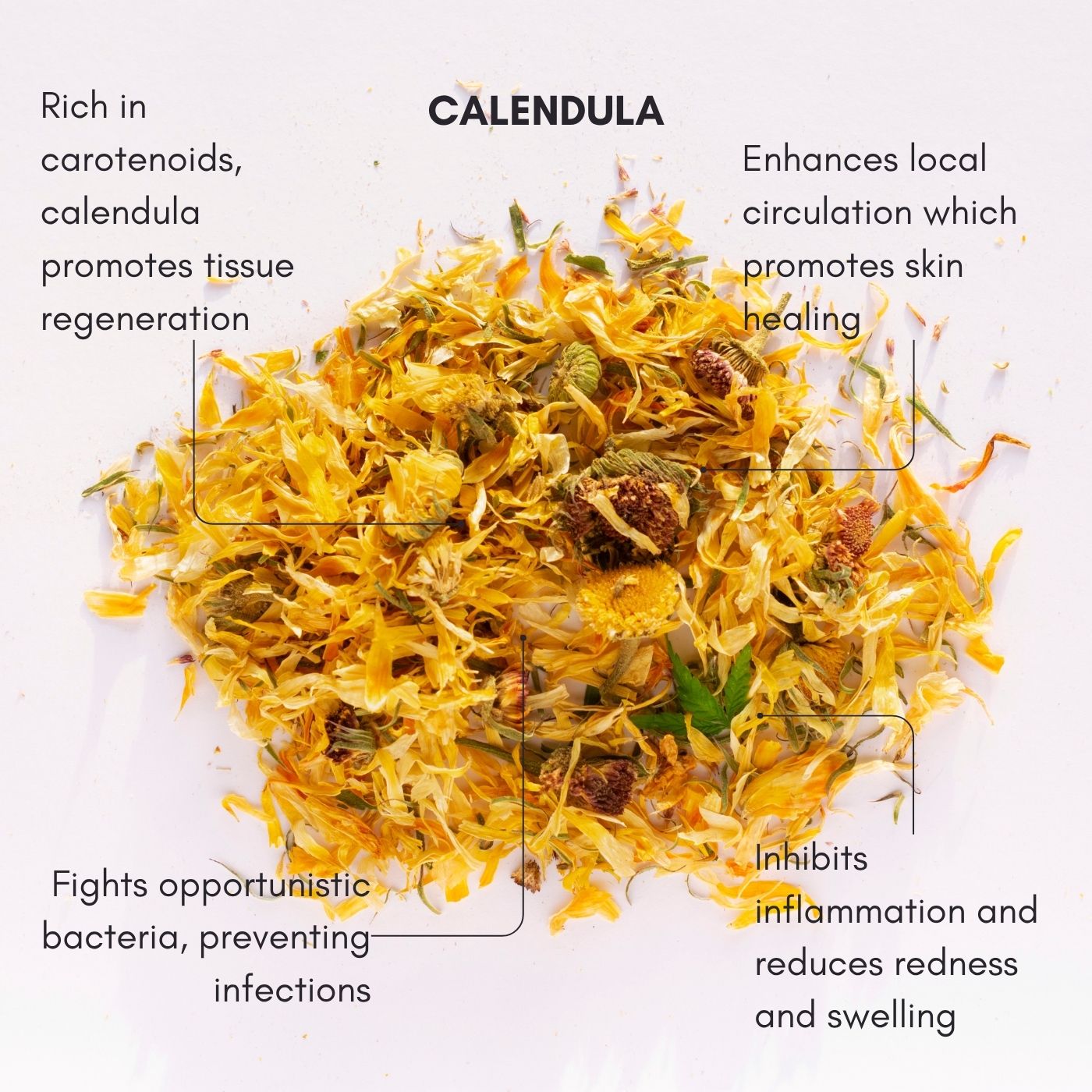
Herbal teas and essential oils provide anti-inflammatory and muscle-relaxing compounds that complement pharmacological approaches. Ginger, cinnamon, and chamomile teas deliver bioactive constituents like gingerol and eugenol, which reduce prostaglandin production and soothe uterine muscles.
Integrating these natural infusions into self-care rituals promotes holistic relief and supports overall well-being.
How do ginger, cinnamon, and chamomile teas reduce period pain?
Infused botanicals contain potent compounds that act on inflammatory pathways:
| Entity | Active Compound | Mechanism | Benefit |
|---|---|---|---|
| Ginger Tea | Gingerol | Inhibits COX enzymes → ↓ Prostaglandins | Lessens cramp intensity and bloating |
| Cinnamon Tea | Cinnamaldehyde | Modulates blood flow → Relaxed muscles | Alleviates spasm-related pain |
| Chamomile Tea | Apigenin | Binds GABA receptors → Calming effect | Reduces tension and promotes relaxation |
Brewing a cup twice daily from 300–500 mg of dried herb can yield noticeable relief before and during menstruation.
What essential oils are effective for menstrual cramp relief and how to use them?
- Lavender Oil: Dilute 2–3 drops in carrier oil; massage onto lower abdomen to promote muscle relaxation.
- Peppermint Oil: Apply a 1% dilution to the lower back for cooling analgesic relief.
- Clary Sage Oil: Inhale from a diffuser to reduce cortisol levels and heighten relaxation.
These application methods harness bioactive terpenes to complement heat therapy and oral remedies.
How does acupressure and acupuncture help reduce menstrual discomfort?
Acupressure and acupuncture target specific meridian points—such as SP6 (Sanyinjiao) and REN4 (Guanyuan)—to modulate nerve inputs, increase endorphin release, and enhance blood flow. Regular sessions or self-massage at these points can lower pain severity and shorten cramp duration by rebalancing energy pathways and reducing inflammation.
Which Dietary Changes and Supplements Support Menstrual Cramps Relief?
An anti-inflammatory diet rich in omega-3 fatty acids, magnesium, and B vitamins addresses systemic inflammation and muscle tension. Combined with adequate hydration, these nutritional strategies fortify uterine health and mitigate prostaglandin-driven contractions.
What anti-inflammatory foods help reduce menstrual cramps?
Incorporate these foods to dampen inflammation naturally:
- Berries (blueberries, strawberries) for anthocyanins
- Leafy greens (spinach, kale) for magnesium and antioxidants
- Fatty fish (salmon, mackerel) for EPA/DHA omega-3s
- Nuts and seeds (walnuts, flaxseeds) for plant-based omega-3s
Adding these anti-inflammatory staples reduces overall prostaglandin synthesis and supports balanced hormone function during menstruation.
How do magnesium, omega-3, and B vitamins ease period pain?
| Entity | Attribute | Value |
|---|---|---|
| Magnesium | Mechanism | Relaxes uterine muscles via calcium regulation |
| Omega-3 | Effect | Inhibits inflammatory prostaglandin pathways |
| Vitamin B6 | Role | Balances hormones and modulates pain signals |
| Vitamin B12 | Benefit | Supports nerve function and energy metabolism |
Typical dosages: magnesium 200–400 mg, omega-3 1000–2000 mg EPA/DHA, and B6 50–100 mg daily. These supplements work synergistically to lower cramp intensity and improve mood during PMS.
Why is hydration important during menstruation for cramp relief?
Adequate water intake prevents tissue dehydration and electrolyte imbalance, which can exacerbate muscle spasms. Staying hydrated maintains optimal blood volume and nutrient delivery to pelvic tissues, further supporting muscle relaxation and reducing bloating that intensifies cramp discomfort.
What Exercises and Lifestyle Changes Can Manage and Prevent Menstrual Cramps?
Regular movement and stress management enhance circulation, raise endorphin levels, and diminish prostaglandin production, creating a holistic foundation for long-term cramp prevention.
Which yoga poses and gentle exercises relieve period pain?
- Child’s Pose (Balasana) – Opens hips and relieves lower-back tension.
- Cat-Cow (Marjaryasana-Bitilasana) – Alternating spinal flexion eases uterine pressure.
- Seated Forward Bend (Paschimottanasana) – Stretches hamstrings to reduce pelvic congestion.
Incorporating 10–15 minutes daily boosts circulation and gradually strengthens supportive musculature.
How does stress reduction impact menstrual cramp severity?
Chronic stress elevates cortisol and inflammatory markers, which can heighten prostaglandin levels and pain sensitivity. Mindfulness meditation, deep-breathing exercises, and progressive muscle relaxation lower stress hormones, reducing uterine hyperactivity and moderating cramp intensity.
Can hormonal birth control help reduce menstrual cramps?
Yes. Combined estrogen-progestin contraceptives suppress ovulation and thin the uterine lining, leading to lower prostaglandin production and lighter periods. Many individuals experience significantly reduced pain severity and duration when on a consistent hormonal regimen.
What Advanced Treatments Are Available for Severe or Secondary Menstrual Cramps?
For persistent or condition-related cramps, targeted medical interventions address underlying pathology—ensuring both symptomatic relief and long-term health.
How do conditions like endometriosis and fibroids cause secondary dysmenorrhea?
Endometriosis implants outside the uterus create inflammatory lesions that respond to hormonal cycles, causing intense, often unilateral pain. Uterine fibroids—benign muscle tumors—distort uterine shape and heighten contractile force, leading to prolonged and severe cramps.
What medical interventions are effective for managing severe menstrual pain?
Clinicians may recommend:
- Hormone-modulating therapies (GnRH agonists, levonorgestrel IUDs) to shrink lesions or fibroids.
- Non-pharmacological devices (TENS units) to deliver electrical pulses that block pain signals.
- Minimally invasive procedures (laparoscopy) to excise endometrial implants.
These options offer deeper relief for underlying causes unresponsive to first-line measures.
When is surgery recommended for menstrual cramps related to underlying conditions?
Surgical interventions become necessary if conservative treatments fail and quality of life declines. Endometriosis excision, myomectomy for fibroids, or hysterectomy in extreme cases restore pelvic anatomy and eliminate the source of secondary dysmenorrhea, providing definitive relief for refractory pain.
Menstrual cramps relief rests on a tailored blend of heat therapy, NSAIDs, natural botanicals, dietary support, and proactive lifestyle changes. Identifying your pain’s root cause—whether prostaglandin-driven contractions or secondary pathology—guides you to the most effective interventions. Integrating heating pads, herbal teas, and evidence-based supplements form a cohesive, multi-modal strategy. For persistent or severe cramps, consult a healthcare professional to explore advanced treatments and ensure comprehensive, long-term comfort.
For a natural, sustainable way to soothe cramps, combine herbal teas, heat therapy, and lifestyle support.
🍵 Try Artemis Period Pain Herbal Beverage — made with carefully selected botanicals that support your cycle and reduce discomfort, the natural way.
















Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.